A case report ofAcute Necrotizing Encephalopathy in a Child
A
2-year-old girl, previously developmentally normal, was brought to the hospital
with a 5-day history of fever, 7 episodes of loose stools per day for 3 days,
and three brief generalized tonic-clonic seizures, accompanied by
encephalopathy and a Glasgow coma scale (GCS) of 9/15. She was initially
treated with ceftriaxone, amikacin, acyclovir, and levetiracetam. Laboratory
tests showed elevated transaminases, ESR, and CRP, while serologies for various
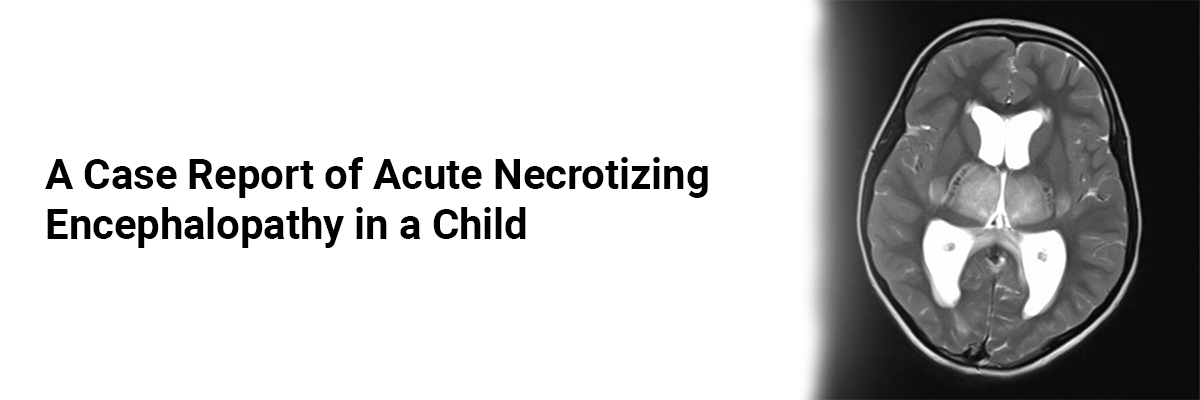
viruses were negative, and CSF analysis was normal. An MRI conducted on the
second day of admission revealed bilateral thalamic hyperintensities with a
'double doughnut' and 'tricolor' pattern. The patient was treated with
intravenous immunoglobulin (IVIG) and methylprednisolone and was discharged on
day 7. Follow-up at two weeks showed her neurological examination to be
unremarkable, with regained ability to walk, understand commands, and speak.
The
case highlights the case of acute necrotizing encephalopathy (ANE), a fulminant, parainfectiousclinico-radiological
syndrome typically showing poor recovery rates. The condition is associated
with cytokine storms due to viral infections and is characterized by specific
neuroimaging findings such as bilateral lesions in the thalamus. Poor outcomes
are linked with factors such as multiorgan dysfunction, low GCS at admission,
and MRI findings.
Source:Bhanudeep
S, Koneti B.B. Successful Management of Acute Necrotizing Encephalopathy in a
Child. Indian J Pediatr. 2025;92(98).
https://doi.org/10.1007/s12098-024-05306-8














Please login to comment on this article