
 IJCP Editorial Team
IJCP Editorial Team
A premature baby with respiratory distress
A report describes a case of an infant female born at 31 weeks of gestation with a weight of 1500 g. She was delivered by cesarean delivery with spinal anesthesia, performed for Sinusoidal Fetal Rhythm (SFR), decreased fetal movements and high Peak Systolic Velocity (PSA) Doppler of both mean cerebral arteries which were firmly suggestive of severe fetal anemia. Her mother was a 26-year-old, gravida 1, para 1, having negative parvovirus serology (IgM and IgG), and uncomplicated pregnancy. Betamethasone was not completed and the mother did not suffer vaginal bleeding. The infant's Apgar scores were 2 at 1 mn, 2 at 5 mn, and 7 at 10 mn. The amniotic liquid was clear.
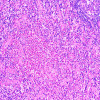
The infant required endotracheal intubation at birth for the absence of respiratory effort after positive-pressure ventilation. Her cord pH was 7.15 and she was flat, had pale skin, and was severely hypoxic. Her heart rate was noted as 122 bpm and the mean blood pressure as 51 mmHg. She was not hydropic. Her hemoglobin was evaluated as 16 mg/dL, platelet count as 100 × 109/L and reticulocytes as 297 × 109/L. She was administered 3 repacked red blood cell transfusions of 10 cc/kg (RBC) and 1 platelet transfusion in the first 12 hours of her life. Her first arterial gas revealed severe metabolic acidosis (PH: 6.87, bicarbonates: 11 mmol/L, base excess: 21, PCO2 60 mmHg, pO2:52 mmHg, and lactates: 15), during which she was on conventional mechanical ventilation with Oxygenation Index of 15 and FiO2 at 100%. Pulmonary hypertension (PPHN) was clinically suspected due to a saturation gradient pre and post-ductal of 10%, which was confirmed by cardiac ultrasound at the bedside. Her first chest x-ray revealed diffuse white lungs bilaterally. She was switched to high-frequency oscillatory ventilation (HFOV) with Mean airway pressure at 16, the amplitude at 25, and frequency at 9 Hertz. Inhaled Nitric oxide (NO) was initiated at 20 ppm with FiO2 of 100%. She received a drip of fentanyl at 1 mcg/kg/h. She was given two doses of surfactant at 1 hour and 5 hours of life without any improvement.
While she was at 100% of FiO2, one dose of muscle paralytic (Rocuronium: 1 mg/kg) was administered to optimize the ventilation and the need for oxygen decreased immediately, reaching progressively 45% at 10 hours of life. Her reports were negative for Toxoplasmosis and Cytomegalovirus (CMV) serology, C reactive protein (CRP), enteroviral and blood cultures, Coombs direct test, and Kleihauer- Betke test.; while normal for Placental examination. Her head ultrasound and renal and liver function were also normal. She was weaned from NO and mechanical ventilation progressively and was extubated 3 days later. Her remaining neonatal period was uneventful and was transferred to a level II hospital at 35 weeks of gestational corrected age. Her clinical examination before the transfer was normal and the hemoglobin level at the discharge time was 109 mg/dl.
Thus, in this case, profound hypoxia persisted despite optimal treatment of classic RDS. The patient responded well to treatment known to be efficacious in pediatric and adult ARDS.
Brahim B, Jean L, Abdelwahab M, Romain M, Ali N. Acute Respiratory Distress Syndrome (ARDS) in Preterm Infants with Severe Fetal Anemia: 2 Case Reports and Review of Literature. Neonat Pediatr Med. 2016; 1: 114. doi:10.4172/2572-4983.1000114

IJCP Editorial Team
Comprising seasoned professionals and experts from the medical field, the IJCP editorial team is dedicated to delivering timely and accurate content and thriving to provide attention-grabbing information for the readers. What sets them apart are their diverse expertise, spanning academia, research, and clinical practice, and their dedication to upholding the highest standards of quality and integrity. With a wealth of experience and a commitment to excellence, the IJCP editorial team strives to provide valuable perspectives, the latest trends, and in-depth analyses across various medical domains, all in a way that keeps you interested and engaged.










Please login to comment on this article