Aortoesophageal Fistula Following Button Battery Ingestion by a Child
A 5-year-old boy was brought to the emergency department with two episodes of hematemesis within the last 5-6 hours.
His parents reported that he had been experiencing vague abdominal discomfort for the previous five days, for which he had received symptomatic treatment from a local practitioner.
On examination, the child showed severe pallor and shock, although the systemic examination was unremarkable.
Shock was managed with a fluid bolus, and he was transferred to the Pediatric Intensive Care Unit (PICU). Endoscopy was planned following a packed red blood cell (PRBC) transfusion.
Blood tests and an abdominal ultrasound were normal, except for anemia and elevated urea levels.
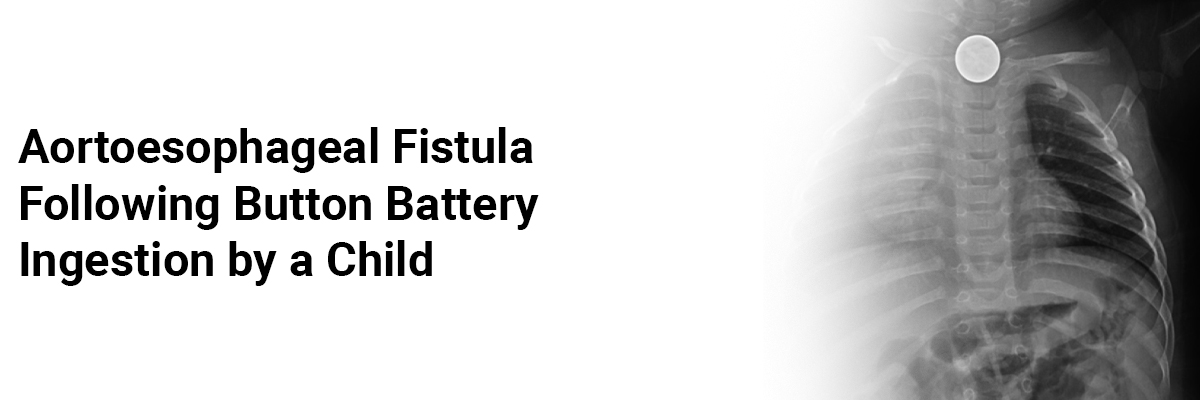
After admission to the PICU, he had a massive hematemesis episode, resulting in hypotension. He was resuscitated with intravenous fluids, PRBCs, inotropes, and mechanical ventilation. A chest radiograph revealed a coin-shaped foreign body with a double ring or halo sign in the mid-thorax. Emergency bedside endoscopy retrieved an impacted esophageal button battery (approximately 20 mm). A CT aortogram indicated an upper lateral esophageal tear and potential aortic injury. Despite aggressive resuscitation, his condition deteriorated, leading to an emergency surgery where a 4 mm necrotic area in the medial wall of the aorta and a corresponding esophageal opening were repaired.
Post-surgery, his condition improved, inotropes were stopped within 24 hours, and he was started on peritoneal dialysis due to multi-organ failure, including acute kidney injury. An endoscopic nasojejunal (NJ) tube was inserted on day 5, and NJ feeds were initiated. He was extubated on day 6 as his recovery progressed. However, on day 12, he experienced another episode of massive hematemesis and hypotension, necessitating thoracotomy. This revealed necrosis of the esophageal and adjoining aortic walls. The esophagus was repaired, and an end-to-end anastomosis of the aorta was performed. Post-surgery, inotropes were tapered, he was extubated after 24 hours, and NJ feeds were resumed. An esophagogram on day 21 showed no tear or leak. He was discharged after a 40-day hospital stay, and at a 1-year follow-up, he showed no signs of esophageal strictures.
Given that many ingestion cases are unwitnessed, considering button battery ingestion in the differential diagnosis of persistent abdominal symptoms is crucial for early diagnosis. A chest and abdomen radiograph can aid in early detection, with the double halo sign distinguishing a battery from a coin.
Button battery ingestions are increasingly recognized as a cause of gastrointestinal bleeding and perforation. Most ingestions are unwitnessed, making diagnosis challenging and highlighting the need for public awareness and safety mechanisms in toys. A thorough history and simple radiographs can confirm the diagnosis.
This case underscores the risk of ongoing injury and severe complications weeks after battery removal, necessitating continued vigilant monitoring. It also emphasizes the importance of a multidisciplinary team in managing and preventing fatal complications from button battery ingestion.
Source: Abraham S, Kurian K, Valliatu J, et al. Indian Pediatrics. 2024 Jun;61(6):597-8.













Please login to comment on this article