Appendectomy During Pregnancy Leading to Abdominal Wound Dehiscence
A 34-year-old woman who was 29 weeks pregnant was brought to the gynecology department of a hospital with two days of lower abdominal pain and elevated inflammatory markers.
The lady exhibited no gastrointestinal symptoms. The current pregnancy had progressed without complications, with normal fetal growth. Her medical history included an uncomplicated vaginal delivery two years prior, no chronic illnesses, and no prior abdominal surgeries.
Acute appendicitis with possible perforation was suspected.
Given the advanced gestational stage, uterine size, and suspected gangrenous peritonitis, a laparotomic approach via McBurney’s incision was selected. Preoperatively, the patient received 3g of intravenous ampicillin/sulbactam as prophylaxis.
Intraoperative findings confirmed appendix perforation with minimal pus in the abdominal cavity. The surgery was completed without complications, with fascia closure and skin sutured with interrupted stitches. A Penrose drain was placed near the cecum.
Postoperatively, fetal viability was confirmed, and magnesium sulfate was administered intravenously for uterine contractions. Hypokalemia was corrected with intravenous potassium. Due to elevated inflammatory markers (WBC: 16 × 10⁹/L; CRP: 225 mg/L), ampicillin/sulbactam 3 g IV every 6 hours was continued.
The patient was started on a dysphagic diet on postoperative day two. However, on day three, she developed a paralytic ileus, requiring a nasogastric tube, central venous catheter, parenteral nutrition, and potassium supplementation.
On day five, inflammatory markers rose again. Cultures identified Escherichia coli (sensitive to all antibiotics) and Pseudomonas aeruginosa (sensitive only to meropenem and amikacin). Antibiotic therapy was adjusted to IV piperacillin/tazobactam 4.5 g and metronidazole 500 mg––which yielded improvement. Greenish fluid from the paracecal drain prompted surgical wound debridement, partial suture removal, and Betadine irrigation.
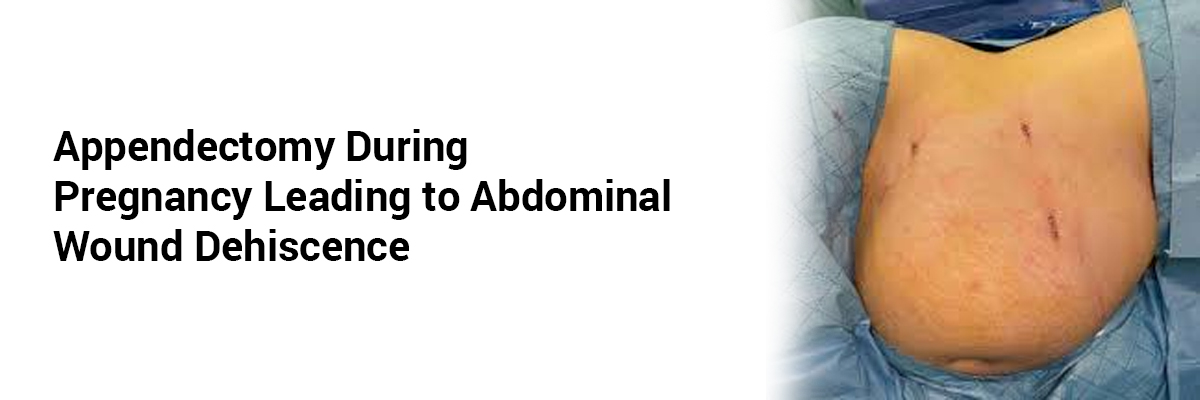
Complete wound dehiscence (9 × 3 cm) with purulent fasciitis and fascia degradation was observed by day eight. The wound exposed the cecum and gravid uterus. After debridement, only the fascia was sutured, and a negative pressure wound therapy (NPWT) system at 50 mmHg was applied. Subsequent hospitalization was uneventful. The patient continued on antibiotics, low-molecular-weight heparin, and magnesium. The heparin was changed every three days under local anesthesia. Six days post-resuture, she was discharged for home care.
The fetus was monitored every week days until the delivery. At 38 weeks and 3 days of gestation, the patient was readmitted due to vaginal bleeding and regular contractions. Three hours after the admission, the patient vaginally delivered a baby boy weighing 2860 g, with an Apgar score of 8-9-9. The lady did not incur any perineal injury, nor did she experience any pain at the NPWT site.
Follow-up included NPWT sponge replacements every 4-6 days and fetal monitoring. On postpartum day three, NPWT was removed under sedation, and the wound was definitively sutured. The healed fascia was covered with granulation tissue, and an EasyFlow drain was inserted before final skin closure. The drain was removed the next day, and the patient was discharged.
At three months postpartum, the wound had healed with a secondary scar. The patient reported no gynecological complications such as dyspareunia or vaginismus, though mild numbness and occasional scar tightness persisted.
This case highlights the importance of NPWT in managing post-appendectomy surgical site infections during pregnancy. Its timely application can prevent preterm birth and enable vaginal delivery. This experience suggests NPWT is both beneficial for the mother and safe for the fetus in extreme cases.
Source: Zapletal J, Sehnal B, Dvorak R, et al. Internl J Gynec & Obst. 2025.















Please login to comment on this article