 IJCP Editorial Team
IJCP Editorial Team
Complicated Acute Pericarditis Caused by Methicillin-Resistant Staphylococcus aureus after Influenza B Virus Infection: A Case Report
A previously healthy 14-month-old girl child visited a local clinic in the winter of 2018 with a 2-day history of high-grade fever and cough on the second day of illness onset. The baby had not received the influenza vaccine that season.
She tested positive for influenza B infection through a rapid antigen-detection test but received no specific treatment at the clinic.
On day 7 of her illness, she was admitted to another hospital due to ongoing fever and cough, where a peripheral venous catheter was inserted. Her chest X-ray revealed no abnormal findings, such as an enlarged heart. She was treated with intravenous rehydration and received prednisolone (1 mg/kg/day) as anti-cytokine therapy through the peripheral vein.
However, her fever, cough, and breathing difficulties worsened. Consequently, on day 9 of her illness, she was hospitalized.
On examination, the baby was conscious but drowsy (Modified Glasgow Coma Scale for infants and children: E2V3M4). Her vital signs were as follows – body temperature, 39.1°C; blood pressure, 92/65 mmHg; heart rate, 158 beats/min; respiratory rate, 65 breaths/min; and oxygen saturation, 99% with O2 at 5 L/min via a mask. She experienced moderate difficulty in breathing, with retractions in the suprasternal and subcostal areas. Her capillary refill time was 3 seconds.
Although there was no pericardial rub, muffled heart sounds were audible during her examination. Additionally, her left lower respiratory sounds were diminished, accompanied by wet rales. There were no signs of jugular venous distension, pedal edema, or pulsus paradoxus. Furthermore, phlebitis was noted at the insertion site of the peripheral venous catheter – in the cephalic vein, characterized by redness, swelling, and a slight purulent discharge.
Laboratory tests revealed abnormal results – a high white blood cell count of 34,200 cells/μL (normal reference values: 4500–13500 cells/μL), with 85.0% neutrophils; a low red blood cell count of 3.61 x 106 cells/μL (normal reference values: 3.76 x 106–5.00 x 106 cells/μL); hemoglobin levels of 8.9 g/dL (normal reference values: 11.3–15.2 g/dL); a hematocrit of 27.0% (normal reference values: 33.4%–44.9%); and a platelet count of 35.9 x 104 cells/μL (normal reference values: 13.1 x 104–36.9 x 104 cells/μL).
Inflammatory biomarkers were elevated, including C-reactive protein (29.75 mg/dL), procalcitonin (1.100 ng/mL), lactate dehydrogenase (453 U/L), creatine kinase (15 U/L), B-type natriuretic peptide (235 pg/mL), and troponin-I (<10 pg/mL).
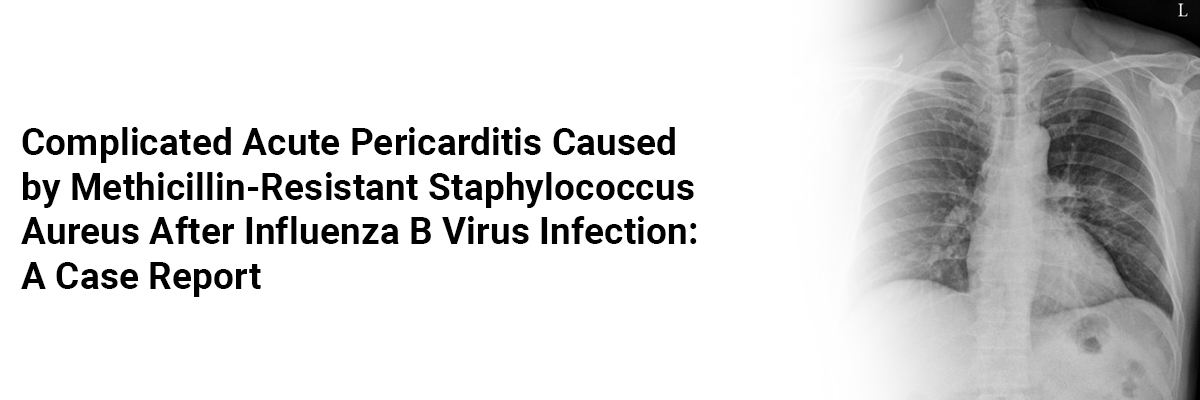
Chest X-rays indicated cardiomegaly, with a cardiothoracic ratio of 0.60. Transthoracic echocardiography revealed pericardial effusion but no respiratory variations, biventricular dysfunction, or global hypokinesia.
Electrocardiography showed PR depression and concave ST elevation in leads II, III, aVF, and V2–V6, along with PR elevation and ST depression in aVR and V1.
A chest computed tomography scan confirmed the presence of pericardial effusion, atelectasis, and pleural effusion in the left lung.
The diagnosis was sepsis, acute pericarditis, and peripheral venous catheter-related bloodstream infection (PVC-BSI). Treatment for acute pericarditis involved administering colchicine, aspirin, and diuretics. Additionally, cefotaxime and vancomycin were initiated due to the blood culture results, which revealed methicillin-resistant Staphylococcus aureus (MRSA). The patient showed improvement after antibiotic treatment, and her symptoms subsided over the following days.
The patient did not experience any complications or recurrences during a four-year follow-up. The antibiotic treatment duration depended on complications related to MRSA infection, and the patient was closely monitored to prevent complications such as cardiac tamponade.
Early identification of the causative organisms and targeted therapy is crucial in children to prevent worsening conditions and mortality due to acute pericarditis. Monitoring the clinical course for potential complications and evaluating treatment outcomes is also essential.
Source: Ochi F, Tauchi H, Miura H, et al. Case Reports in Pediatrics. 2023 May 2;2023.

IJCP Editorial Team
Comprising seasoned professionals and experts from the medical field, the IJCP editorial team is dedicated to delivering timely and accurate content and thriving to provide attention-grabbing information for the readers. What sets them apart are their diverse expertise, spanning academia, research, and clinical practice, and their dedication to upholding the highest standards of quality and integrity. With a wealth of experience and a commitment to excellence, the IJCP editorial team strives to provide valuable perspectives, the latest trends, and in-depth analyses across various medical domains, all in a way that keeps you interested and engaged.





















Please login to comment on this article