 IJCP Editorial Team
IJCP Editorial Team
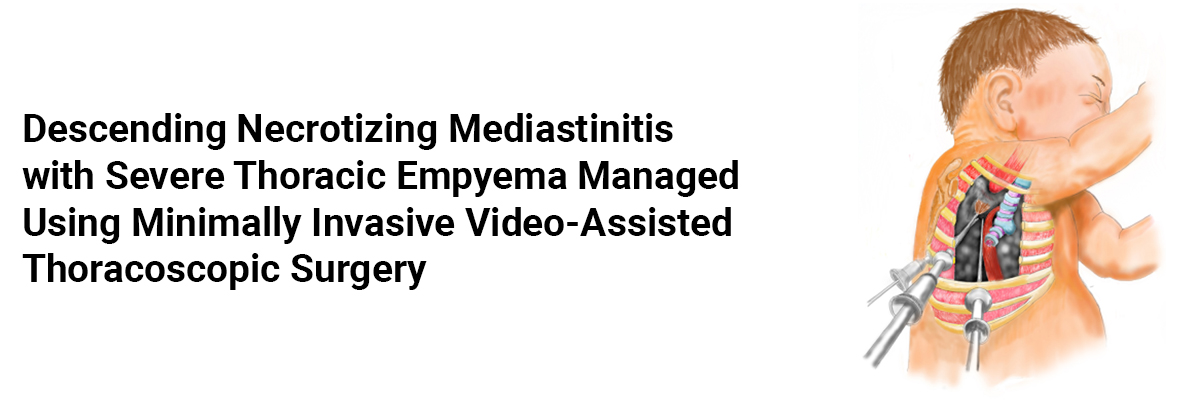
Descending necrotizing mediastinitis with severe thoracic empyema managed using minimally invasive video-assisted thoracoscopic surgery
A report describes a case of a 6-year-old previously healthy girl who presented with odynophagia and dental pain of the right upper molars. One day later, she got hospitalized with a high fever of 40 ℃. Despite administering broad-spectrum antibiotics, her fever persisted. On the fourth day, her dental pain gradually resolved, but tachypnea and left chest pain evolved. An urgent chest computed tomography (CT) demonstrated pneumonia, pleural effusion, widening of the mediastinum, and air bubbles accumulation in the neck. She was then transferred immediately to another facility for intensive care.
On admission, her temperature was 38.6 ℃, pulse rate was 138 beats/min, respiratory rate was 40 breaths/min, blood pressure was 114/69 mmHg, and pulse oximetry was 95% on room air. She displayed no redness, localized swelling, or enlarged lymph nodes on her neck.
She received empirical treatment with meropenem (60 mg/kg per day) and linezolid (30 mg/kg per day). Yet, her tachypnea and dyspnea progressed rapidly.
An ultrasound-guided left-sided thoracentesis drained 80 mL of brown sticky pus on the second day in the recent healthcare facility. The laboratory examinations of the drained fluid revealed low glucose, high protein levels, and neutrophil predominance. Pus culture for only aerobes showed Streptococcus constellatus, and the blood culture came negative.
On the third day, a contrast-enhanced CT scan of the neck and chest was compared with her previous CT scan result, which revealed enlargement of an area of the mediastinal abscess and increased severity of thoracic empyema. Air and fluid rapidly extended to the upper mediastinum and accumulated in this region. However, the low-density area of the abscess encircling the right common carotid artery in the neck diminished. The patient thus received a diagnosis of descending necrotizing mediastinitis (DNM) complicated with severe empyema on the left side.
She underwent VATS for left thoracic and mediastinal drainage under general endotracheal anesthesia with two-lung ventilation the next day, which led to the surgical debridement of the mediastinum and pleura with complete excision and decortication of necrotic tissue. Her Drainage cultures came negative.
The patient's fever resolved within three days of surgery. Her drains were removed on hospital day 10, and on the same day, the C-reactive protein (CRP) level decreased to 7.9 mg/L. She was switched from meropenem to ceftazidime at 100 mg/kg daily for stepping-down antibiotic therapy.
The patient fully recovered and received a discharge without any complications on hospital day 18 after near-normal mediastinal contours were confirmed with chest radiography.
Zhang Y, Wang W, Xin X, Jin Y, Liu W, Du G, Guo F. Management of descending necrotizing mediastinitis with severe thoracic empyema using minimally invasive video-assisted thoracoscopic surgery: a case report. Transl Pediatr 2022;11(8):1415-1421. doi: 10.21037/tp-22-60

IJCP Editorial Team
Comprising seasoned professionals and experts from the medical field, the IJCP editorial team is dedicated to delivering timely and accurate content and thriving to provide attention-grabbing information for the readers. What sets them apart are their diverse expertise, spanning academia, research, and clinical practice, and their dedication to upholding the highest standards of quality and integrity. With a wealth of experience and a commitment to excellence, the IJCP editorial team strives to provide valuable perspectives, the latest trends, and in-depth analyses across various medical domains, all in a way that keeps you interested and engaged.




















Please login to comment on this article