 IJCP Editorial Team
IJCP Editorial Team
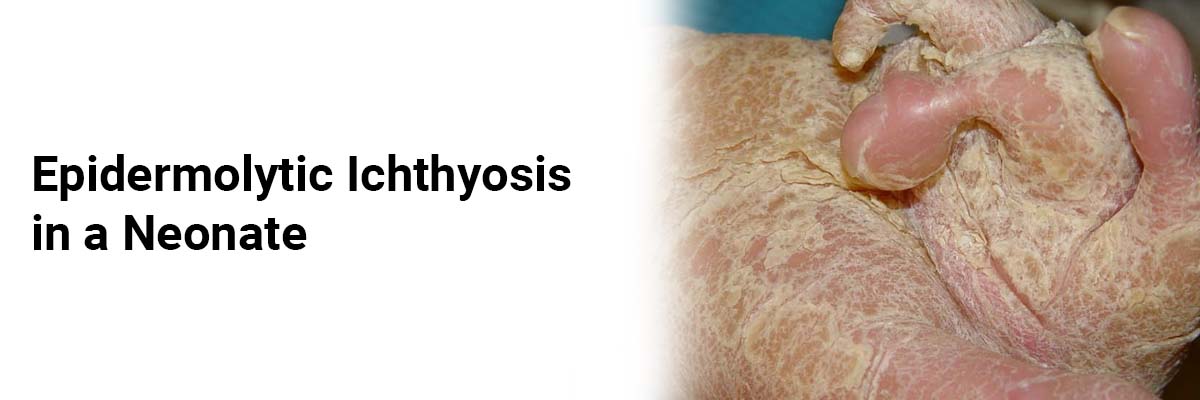
Epidermolytic Ichthyosis in a Neonate
The
parents of a two-week-old male reported dry and cracked skin of the neonate,
noticed at birth.
The baby
had no prior medical history. Shortly after birth, he developed superficial
bullae following minor skin trauma. These bullae occurred on the knees, elbows,
and ankles, resolving quickly without apparent discomfort.
Genetic
testing confirmed a diagnosis of epidermolytic ichthyosis (EI) caused by a
mutation in the KRT10 gene. The initial examination revealed raw erosions on
the left areola and a single tense bulla on the right leg, among other skin
abnormalities.
At the
one-month follow-up, topical petrolatum-based emollients significantly improved
overall skin fragility and blistering.
Epidermolytic
ichthyosis is part of the ichthyosis dermatoses family, characterized by
abnormal cell turnover and epidermal dysfunction. It was formerly known as
epidermolytic hyperkeratosis, a bullous congenital ichthyosiform erythroderma
subtype. EI results from mutations in the KRT1, KRT2, and KRT10 genes,
responsible for keratin intermediate filament formation. This patient exhibited
a de
novo mutation, as there was no family history of EI.
Diagnosing
EI in neonates can be challenging, with differential diagnoses including
epidermolysis bullosa and Staphylococcal scalded skin syndrome. Clinical
features include diffuse erythroderma, superficial bullae, and erosions within
the first week of life. As infants with EI are prone to electrolyte imbalances,
sepsis, and complications, careful monitoring is essential.
Protective measures such as gentle physical contact, moisturizing, and avoiding adhesive dressings are recommended. In childhood, treatments may include topical tretinoin, emollients, and keratolytics, with caution advised for oral retinoids due to potential adverse effects on epidermal fragility and lesion exacerbation.
Source: Pan S, Leszczynska MA, Parekh P, Hendrick SJ. The Journal of Pediatrics. 2023 Dec 1;263.

IJCP Editorial Team
Comprising seasoned professionals and experts from the medical field, the IJCP editorial team is dedicated to delivering timely and accurate content and thriving to provide attention-grabbing information for the readers. What sets them apart are their diverse expertise, spanning academia, research, and clinical practice, and their dedication to upholding the highest standards of quality and integrity. With a wealth of experience and a commitment to excellence, the IJCP editorial team strives to provide valuable perspectives, the latest trends, and in-depth analyses across various medical domains, all in a way that keeps you interested and engaged.






















Please login to comment on this article