 IJCP Editorial Team
IJCP Editorial Team
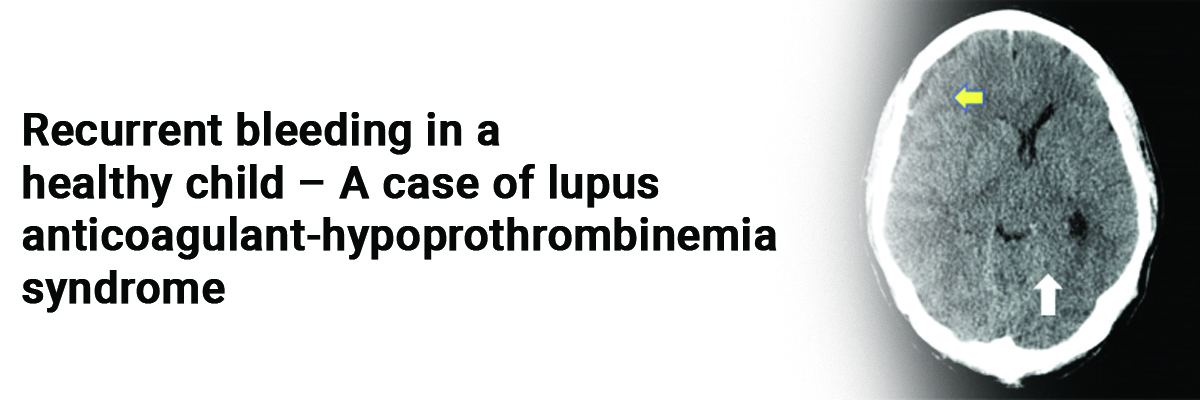
Recurrent bleeding in a healthy child – A case of lupus anticoagulant-hypoprothrombinemia syndrome
A 9-year-old boy was admitted to the pediatric ward due to an acute swelling in the left popliteal fossa. The swelling was first observed about 2 weeks back and had progressed.
In addition, the child had also noted swelling in the left great toe for the past 3 days.
A recent fever, cough, trauma, drug intake episodes, a history of facial rash, oral mucosal lesions, or dactylitis were absent. The boy had a history of recurrent painful joint swellings since the age of 6 months, accompanied by spontaneous subsiding ecchymotic skin patches. There was no history of epistaxis, melena, or blood product transfusions.
On examination, the child was in stable condition, afebrile, with normal height and body mass index (BMI). There were no signs of pallor or lymphadenopathy. Systemic examination revealed no hepatosplenomegaly or arthritis. The left popliteal fossa appeared swollen and had a shiny bluish patch on the skin. The left great toe was also swollen and tender.
Based on these findings, the provisional diagnoses considered were a bleeding disorder, sickle cell disease, connective tissue disorder, or systemic juvenile rheumatoid arthritis.
Laboratory tests showed a hemoglobin (Hb) level of 9.8 mg/dL, total leukocyte count (TLC) of 11,500/cmm, platelet count of 2.62 lakh/cmm, and slightly elevated inflammatory markers. Liver and kidney function tests were within normal limits. Viral screenings for HIV and hepatitis B were negative. The child had prolonged prothrombin time (PT) and activated partial thromboplastin clotting time (APTT), but normal bleeding and clotting times. Further investigations revealed a low prothrombin level, high partial thromboplastin time-LA specific (PTT-LA), and LA antibodies. Von Willebrand factor (VWF) collagen binding was slightly elevated, while other coagulation factors were normal.
The clinical presentation and abnormal coagulation parameters suggested the possibility of Lupus Anticoagulant-Hypoprothrombinemia Syndrome (LA-HPS).
The patient was prescribed prednisolone. The intervention caused complete recovery, with subsequent normal coagulation test results.
However, the boy experienced a relapse with petechial patches after 3 months, which again responded well to prednisolone treatment.
Ultimately, he was diagnosed with persistent primary LA-HPS, a rare cause of bleeding in children.
Raising awareness of this condition can aid in its early diagnosis through appropriate testing, such as prothrombin levels and LA antibody screening.
Source: Kumar S, Bhattacharya P, Gautam S, Chattopadhyay N. Indian Pediatrics Case Reports. 2023 Jul 1;3(3):134.

IJCP Editorial Team
Comprising seasoned professionals and experts from the medical field, the IJCP editorial team is dedicated to delivering timely and accurate content and thriving to provide attention-grabbing information for the readers. What sets them apart are their diverse expertise, spanning academia, research, and clinical practice, and their dedication to upholding the highest standards of quality and integrity. With a wealth of experience and a commitment to excellence, the IJCP editorial team strives to provide valuable perspectives, the latest trends, and in-depth analyses across various medical domains, all in a way that keeps you interested and engaged.




















Please login to comment on this article