Ruptured exophytic uterine artery pseudoaneurysm manifesting a week after vaginal delivery: A case report
A 31-year-old postpartum womanwas hospitalized eight days after delivery due to worsening abdominal pain.
She had no history of vascular disease or significant medical, gynecological, or surgical history. Her pregnancy had been uneventful – vaginal delivery at 39 weeks and 2 days. Labor was augmented with oxytocin and uterine fundal pressure due to arrested labor. The first stage lasted 11 hours and 20 minutes, and the second stage lasted 48 minutes. Blood loss was 200 mL. The infant weighed 3,710 g and had Apgar scores of 1 at 1 minute and 5 at 5 minutes, with an umbilical artery pH of 7.08. The patient was initially discharged without complications. However, on the seventh day postpartum, she developed persistent abdominal pain and fever.
Antibiotic treatment with imipenem-cilastatin and isepamicin sulfate was administered at the referral hospital. She was transferred to the tertiary center on the eighth day postpartum when her symptoms did not improve.
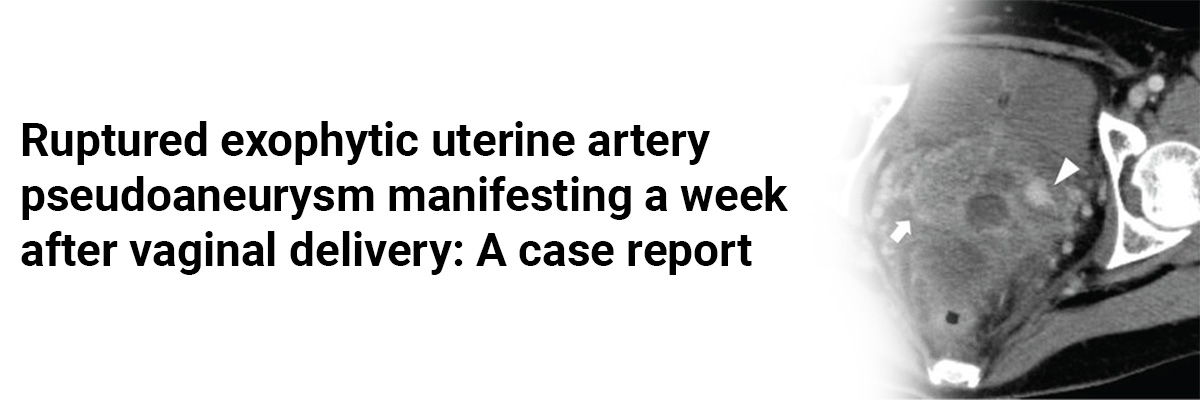
Upon admission, she was hemodynamically stable with no vaginal bleeding. Laboratory tests showed a white blood cell count of 11.7 x 103/μL, C-reactive protein level of 14.8 mg/dL, and hemoglobin level of 9.4 g/dL. Vaginal and blood cultures rendered negative results. Transvaginal ultrasonography identified a hypoechoic mass (17.6 x 16.7 mm) near the left cervicocorporeal junction within an 8 cm hematoma, with turbulent swirling flow suggesting an exophytic uterine artery pseudoaneurysm (UAP) with hemoperitoneum. Contrast-enhanced computed tomography confirmed a ruptured exophytic UAP originating from the left uterine artery. Selective left iliac angiography via the right femoral artery revealed a pseudoaneurysm at the left uterine artery bifurcation, with contrast extravasation.
Embolization was performed using n-butyl-2-cyanoacrylate (NBCA) and coils, resolving her abdominal pain immediately. Follow-up ultrasonography showed a thrombosed pseudoaneurysm with no further hemoperitoneum. Magnetic resonance imaging two days later indicated a hematoma from the thrombosed UAP to the abdominal cavity – suggesting a laceration in the left broad ligament. There was no uterine rupture or abnormality. Without signs of hereditary connective tissue disease, the hemoperitoneum gradually subsided.
Given the persistent fever, tazobactam/piperacillin was administered for ten days to address possible sepsis, after which the fever resolved. The patient was discharged 12 days post-embolization. An eight-month follow-up was uneventful, with no UAP visible on transvaginal ultrasonography.
Postpartum fever and abdominal pain strongly indicate a ruptured exophytic UAP. An exophytic UAP can rupture shortly after delivery without specific risk factors. Obstetricians should be aware of this possibility to ensure early diagnosis and management.
Source: Toshimitsu M, Iriyama T, Sato J, et al. Case Reports in Obstetrics and Gynecology. 2023 Nov 25;2023.















Please login to comment on this article