 IJCP Editorial Team
IJCP Editorial Team
Urachal Anomalies during Infancy
The first case: A preterm female with a delayed umbilical cord detachment underwent abdominal ultrasonography that displayed a 24 mm hypoechoic tract extending from the umbilicus to the bladder. Surgical exploration identified a urachal remnant, leading to excision and umbilicoplasty with a successful recovery.
The second case: An 18-day-old was diagnosed with omphalitis, exhibiting a wide and wet appearance. Ultrasonography revealed a 29.4 mm inflamed hypoechoic tract from the umbilicus to the bladder, diagnosed as a complicated urachal sinus. Surgical excision and drainage were performed, with subsequent improvement on antibiotics.
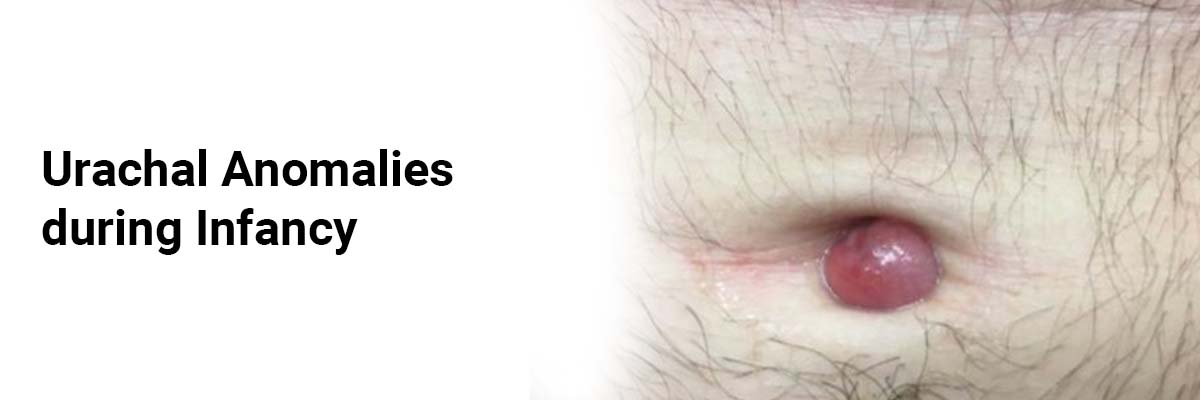
The third and the fourth cases were identified during routine visits at 6 weeks. Both presented with peculiar umbilical appearances confirmed by ultrasound as urachal anomalies. They were conservatively managed.
The fifth case: A late preterm with purulent umbilical discharge and a polypoid structure, underwent ultrasonography revealing a small urachal sinus, managed conservatively.
The sixth case: A one-year-old boy with intermittent umbilical discharge exhibited a wet and erythematous umbilicus. Ultrasonography identified a well-defined urachal cyst. He was treated with a short course of oral antibiotics.
The seventh case: A 4-week-old neonate was brought for a routine checkup. The boy displayed an inguinoscrotal swelling. A scan was immediately conducted, which revealed a small urachal sinus.
A thorough examination revealed a small polypoid structure at the base of the umbilicus.
Urachal anomalies are frequently observed in asymptomatic children, with abdominal ultrasonography revealing them in 99% of cases. However, a population-based study from Canada noted urachal remnants in 1% of screened patients, with a male preponderance. Typically, these anomalies are discovered incidentally, and clinical presentation varies based on factors such as size, location, and age of the patient. While a patent urachus is usually evident at birth, other anomalies may be asymptomatic or present later in life with symptoms ranging from umbilical discharge to abdominal discomfort.
Urachal anomalies appear as luminal hypoechoic structures visualized until the bladder level, while the normal obliterated urachal remnant appears as a non-luminal fibrous grey band. Infections are the most common complication, and surgical intervention is often recommended to avoid potential risks.
Despite the recent preference toward a conservative approach for most urachal anomalies, surgical intervention is still advised due to the risk of complications, recurrent infection, and potential malignant transformation. Spontaneous regression has been reported in cases younger than 6 months – supporting conservative management in these instances.
The risk for malignant transformation, particularly adenocarcinoma, is low, justifying elective excision in specific cases. Abnormal umbilical appearance may serve as an indicator of underlying anomalies, emphasizing the importance of screening ultrasound and thorough evaluation of the genitourinary tract.
The initial management should involve observation, regardless of presentation, with follow-up every 3-6 months until 5 years to detect complications early. Early detection supports timely elective surgery if a conservative approach proves ineffective.
Source: Rustogi D, Panwar JB, Motla M, Kumar K. Indian
Pediatrics. 2023 Oct;60(10):863-5.

IJCP Editorial Team
Comprising seasoned professionals and experts from the medical field, the IJCP editorial team is dedicated to delivering timely and accurate content and thriving to provide attention-grabbing information for the readers. What sets them apart are their diverse expertise, spanning academia, research, and clinical practice, and their dedication to upholding the highest standards of quality and integrity. With a wealth of experience and a commitment to excellence, the IJCP editorial team strives to provide valuable perspectives, the latest trends, and in-depth analyses across various medical domains, all in a way that keeps you interested and engaged.





















Please login to comment on this article